SAI360 FOR HEALTHCARE REVENUE INTEGRITY DIRECTORS
Reducing revenue leaks, improving reimbursements and eliminating issues of non-compliant billing requires effective processes and controls. That’s why you need an efficient, focused program for claims audit and denials management that brings revenue integrity full circle.
Prevent denials
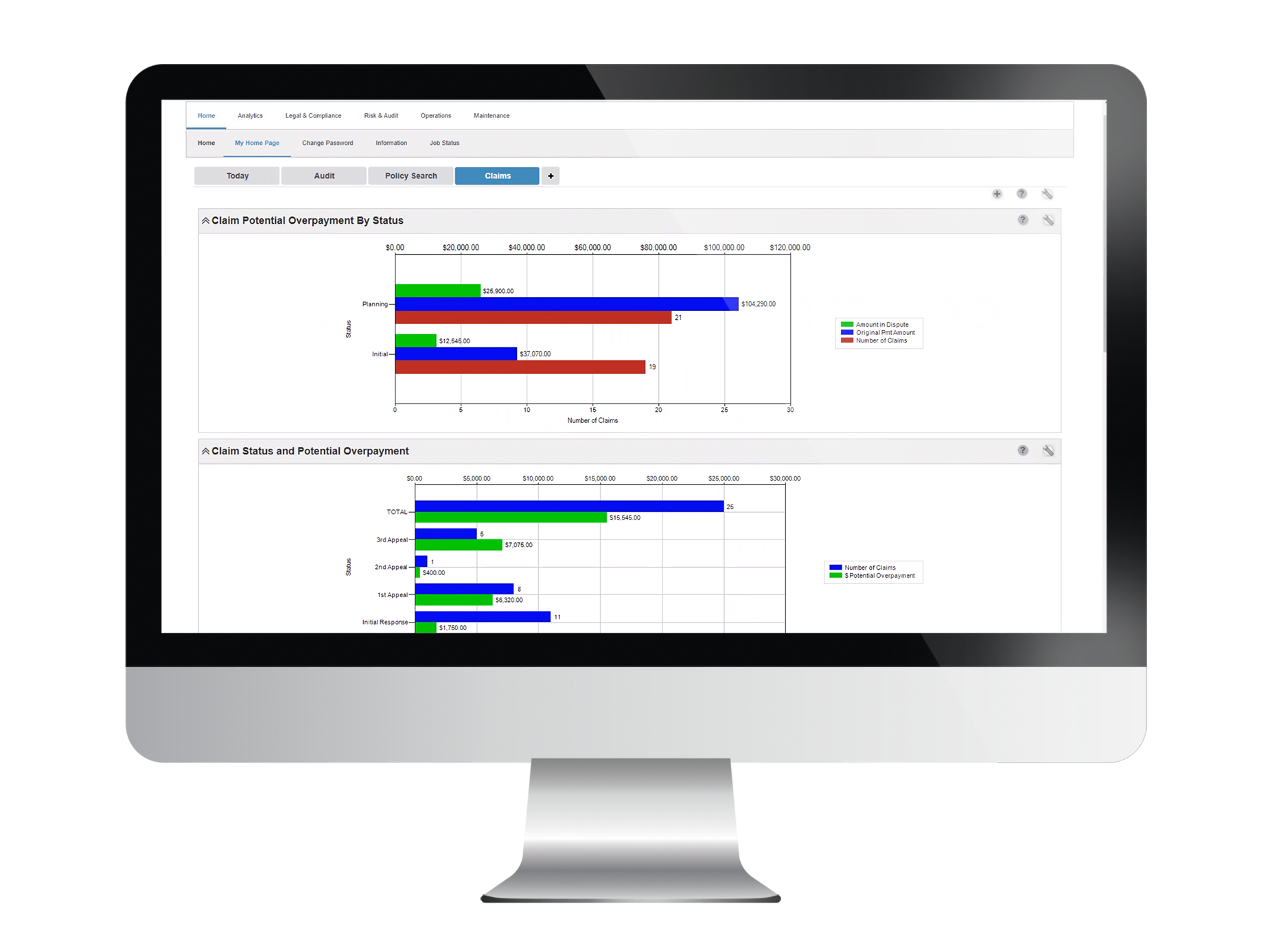
- Visibility into root causes of denials from physicians, service lines, payers and more
- Real-time, actionable intelligence for a 360° view of financial exposure
- Continuous monitoring of claims remittances to detect at-risk payments
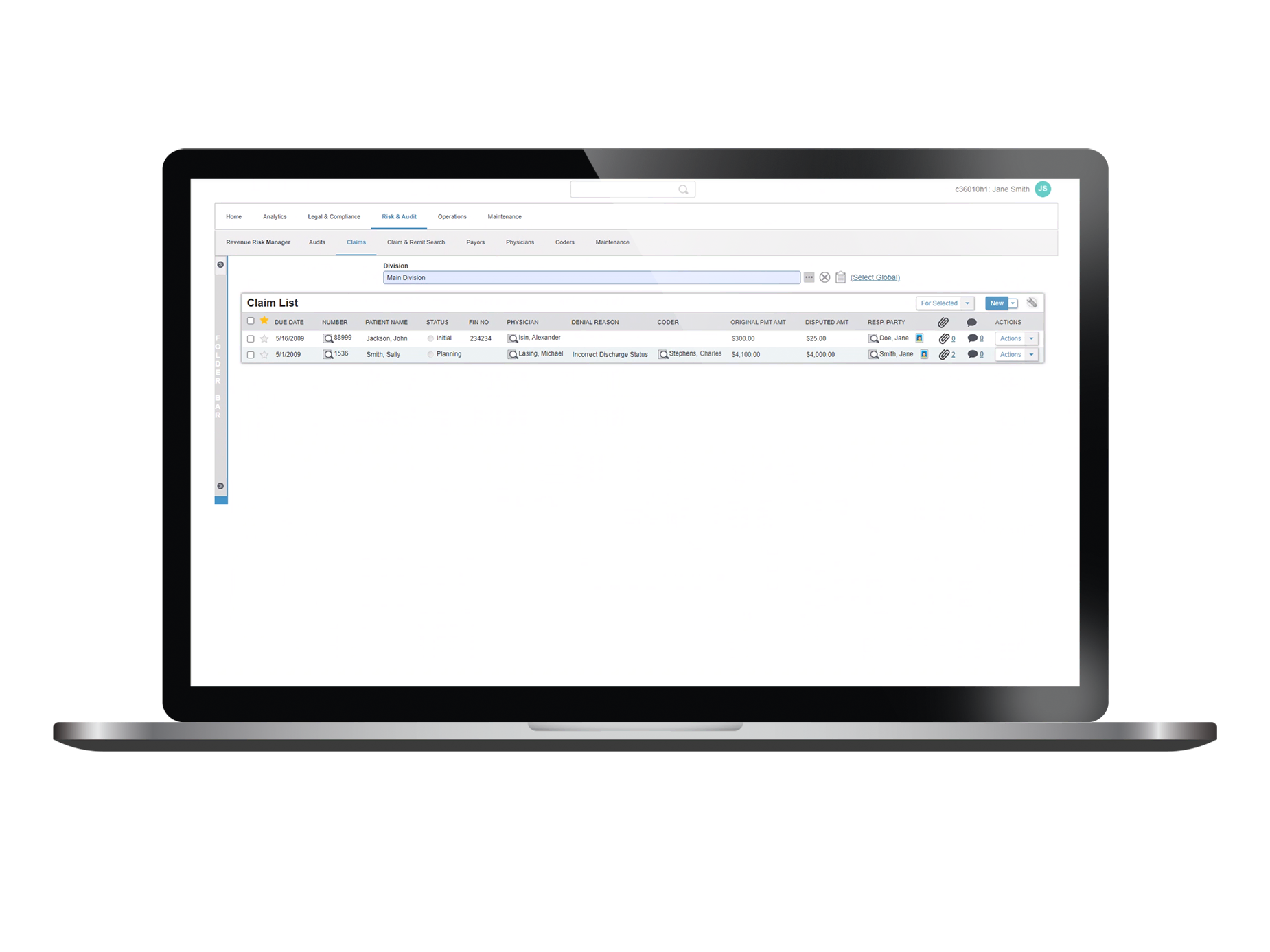
- Configurable workflows that route denied claims through entire audit and appeal process
Stay ahead of payer audits
- Improved auditing of claims data to reduce billing errors and improve reimbursements
- Enhanced data and information sharing across all stakeholders
- Efficient, timely responses and appeals
- Automatic detection and notification of documentation requests from CMS FISS
Promote revenue integrity
- Secure and efficient management of claims denials and payer audits
- Increased transparency and accountability across multi-functional teams
- Effortless reporting to leadership on denial trends and financial exposure
Explore Healthcare Revenue Integrity Management on the SAI360 platform




