SAI360 Healthcare to Detect and Prevent Telehealth Fraud
Identify risks and protect your healthcare organization from the penalties and complexities of telehealth fraud and abuse.
Telehealth adoption has increased significantly. Digital contact with payers and providers has also increased, with a large percentage of members saying they connected with their healthcare providers via web, mobile applications, or text messages. With this spike in telemedicine and other efforts to modernize healthcare delivery over a short period of time, there is a high potential for mistakes, waste, abuse and fraud to occur, which pose significant audit and financial risks to healthcare and health insurance organizations.
SAI360 Healthcare is a configurable software solution that enables you to stay organized, mitigate risks and prevent fines and penalties. Our automated risk management and compliance software enables your team to prepare for regulatory changes, updates and risks as use of mobile healthcare increases.
The SAI360 Telehealth Fraud Essentials solution organizes disparate repositories of contracts and agreements and numerous physician arrangements with vendors and service providers. It has built-in tools to manage multiple appeals processes, response timelines and documentation requirements, which can help protect your organization during regulatory review.
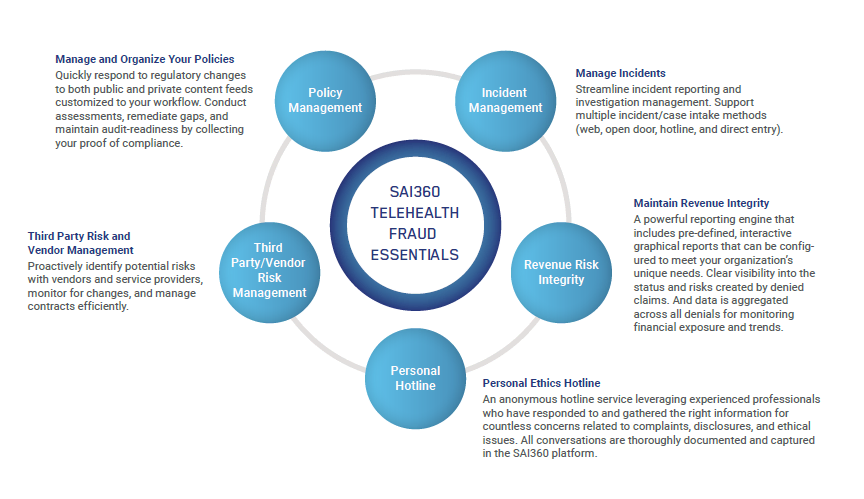 |
Included in the SAI360 Telehealth Fraud Essentials are policy, incident, third-party management, and revenue risk management software modules, as well as a built-in customized hotline. Your organization benefits from coordinated oversite of the multiple vendors involved in providing telehealth services to your patients and healthcare community.
- Manage and Organize Your Policies — Quickly respond to regulatory changes to both public and private content feeds customized to your workflow. Conduct assessments, remediate gaps and maintain audit readiness by collecting your proof of compliance.
- Manage Incidents — Streamline incident reporting and investigation management with support for multiple incident/case intake methods (web, open door, hotline and direct entry).
- Maintain Revenue Integrity — Take advantage of a powerful reporting engine that includes pre-defined, interactive graphical reports that can be configured to meet your organization’s unique needs. Gain clear visibility into the status and risks created by denied claims, and review data that is aggregated across all denials for monitoring financial exposure and trends.
- Third-Party Risk and Vendor Management — Proactively identify potential risks with vendors and service providers, monitor for changes and manage contracts efficiently.
- Personal Ethics Hotline Number — An anonymous hotline service leveraging experienced professionals who gather and respond to the right information for countless concerns related to complaints, disclosures and ethical issues. All conversations are documented and captured in the SAI360 platform.
Contact us for details on our integrated risk management approach to telehealth fraud detection and prevention.
Hear from the healthcare compliance experts
Replay our recent expert panel webinar to learn about the key challenges and approaches to addressing telehealth fraud, featuring Jay Ostrowski (Adaptive Telehealth), Matt Kelly (Radical Compliance), Giovanni Gallo (ComplianceLine), and Tera Peterson (SAI360).
Learn more about our risk management and compliance solutions for healthcare and health insurance organizations.



